25 mcg
orange
Make sure dosing is tailored to every patient 12 precise dosing options
With careful titration, Synthroid can help manage your patient's hypothyroidism. Synthroid should be taken as a single daily dose.1
50 mcg
white
75 mcg
violet
88 mcg
olive

100 mcg
yellow
112 mcg
rose

125 mcg
brown
137 mcg
turquoise

150 mcg
blue

175 mcg
lilac

200 mcg
pink

300 mcg
green
Tablets shown not actual size and may not represent actual color.
Download a brochure about how to take Synthroid correctly to share with your patients
Hypothyroid medications require precise dosing and careful monitoring
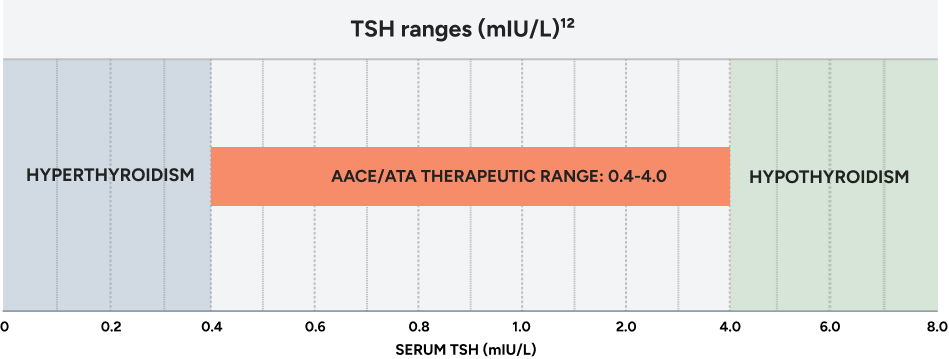
Thyroid disease spectrum
The goal is to achieve steady TSH levels within the appropriate therapeutic range.
Abbreviations: AACE, American Association of Clinical Endocrinologists; ATA, American Thyroid Association; NACB, National Academy of Clinical Biochemistry.
TSH levels alone may not be diagnostic of a thyroid disorder. Additional laboratory testing and clinical findings may be necessary.
Starting dose calculator for adults
Healthy, nonpregnant, non-elderly adults not at risk of disease
Dosing must be individualized based on your patient’s age, weight, cardiovascular status, concomitant medical conditions (including pregnancy), concomitant medications, co-administered food, and the specific etiology of the condition being treated.2 See full prescribing information for dosing in specific patient populations.1
<!-- html container -->
Tablets shown not actual size and may not represent actual color.
Synthroid dosing chart for primary hypothyroidism with adult dosing considerations1
| Patient Population | Starting Dose | Dose Adjustment & Titration |
|---|---|---|
| Adults diagnosed with hypothyroidism | Full replacement dose is 1.6 mcg/kg/day. Some patients require a lower starting dose. | Titrate dosing by 12.5 to 25 mcg increments every 4 to 6 weeks as needed until the patient is euthyroid. |
| Adults at risk for atrial fibrilation or with underlying cardiac disease | Lower starting dose (less than 1.6 mcg/kd/day) | Titrate dosage every 6 to 8 weeks, as needed until the patient is euthyroid. |
| Geriatric patients | Lower starting dose (less than 1.6 mcg/kg/day) | Titrate dosage every 6 to 8 weeks, as needed until the patient is euthyroid. |
| Pregnant patients with pre-existing primary hypothyroidism with serum TSH above normal trimester-specific range | Pre-pregnancy dosage may increase during pregnancy | Increase Synthroid dosage by 12.5 to 25 mcg per day. Monitor TSH every 4 weeks until a stable dose is reached and serum TSH is within normal trimester-specific rage. Reduce Synthroid dosage to pre-pregnancy levels immediately after delivery. Monitor serum TSH 4 to 8 weeks postpartum. |
| Pregnant patients with new onset hypothyroidism (TSH ≥10 mIU per liter) | 1.6 mcg/kg/day | Monitor serum TSH every 4 weeks and adjust Synthroid dosage until serum TSH is within normal trimester-specific range. |
| Pregnant patients with new onset hypothyroidism (TSH <10 mIU per liter) | 1.0 mcg/kg/day | Monitor serum TSH every 4 weeks and adjust Synthroid dosage until serum TSH is within normal trimester-specific range. |
- The dosage of Synthroid depends on a variety of factors including: the patient's age, body weight, cardiovascular status, concomitant medical conditions (including pregnancy), concomitant medications, co-administered food, and the specific nature of the condition being treated.
- Dosing must be individualized to account for these factors and dosage adjustments made based on periodic assessment of the patient's clinical response and laboratory parameters.
- Exercise caution with administering to patients with underlying cardiovascular disease, the elderly, and those with concomitant adrenal insufficiency.
- For pregnant patients with pre-existing hypothyroidism, measure serum TSH and free-T4 as soon as pregnancy is confirmed and, at minimum, during each trimester of pregnancy. In pregnant patients with primary hypothyroidism, maintain serum TSH in the trimester-specific reference range.
- If you have a patient who is taking biotin, tell them to discontinue it at least 2 days before assessing TSH and other thyroid function tests.
Discuss the following with patients when prescribing Synthroid
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1
25 mcg
orange
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1
50 mcg
white
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1
75 mcg
violet
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1
88 mcg
olive
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1

100 mcg
yellow
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1
112 mcg
rose
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1

125 mcg
brown
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1
137 mcg
turquoise
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1

150 mcg
blue
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1

175 mcg
lilac
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1

200 mcg
pink
Select the dose from below and see the pill above
- Since substitutions can be made at the pharmacy, it’s important that you discuss with patients what their Synthroid pill looks like.
- Remind them that only Synthroid has the name "Synthroid" embossed on every pill and that each dose has a specific color.1
- Synthroid is taken as a single daily dose, taken on an empty stomach, 30 minutes to 1 hour before breakfast.1

300 mcg
green
Select the dose from below and see the pill above
The FDA has determined that certain levothyroxine products are therapeutically equivalent, and can be substituted at the pharmacy with the full expectation that the substituted product will produce the same clinical effect and safety profile as the reference product.9
Tablets shown not actual size and may not represent actual color.
Download a PDF of the “How to take Synthroid” brochure to share with your patients
Drugs that may decrease T4 absorption (hypothyroidism)
Potential impact: Concurrent use may reduce the efficacy of Synthroid by binding and delaying or preventing absorption, potentially resulting in hypothyroidism.1
| Drug or Drug Class | Effect |
|---|---|
| Phosphate Binders (eg, calcium carbonate, ferrous sulfate, sevelamer, lanthanum) | Phosphate binders may bind to levothyroxine. Administer Synthroid at least 4 hours apart from these agents. |
| Orlistat | Monitor patients treated concomitantly with orlistat and Synthroid for changes in thyroid function. |
| Bile Acid Sequestrants (eg, colesevelam, cholestyramine, colestipol) | Bile acid sequestrants and ion exchange resins are known to decrease levothyroxine absorption. Administer Synthroid at least 4 hours prior to these drugs or monitor TSH levels. |
| Ion Exchange Resins (eg, Kayexalate) | Ion exchange resins are known to decrease levothyroxine absorption. Administer Synthroid at least 4 hours prior to these drugs or monitor TSH levels. |
| Proton Pump Inhibitors, Sucralfate, Antacid (eg, aluminum & magnesium hydroxides, simethicone) | Gastric acidity is an essential requirement for adequate absorption of levothyroxine. Sucralfate, antacids, and proton pump inhibitors may cause hypochlorhydria, affect intragastric pH, and reduce levothyroxine absorption. Monitor patients appropriately. |
Drugs that may alter T4 and triiodothyronine (T3) serum transport without affecting free thyroxine (FT4) concentration (euthyroidism)1
| Drug or Drug Class | Effect |
|---|---|
| Clofibrate Estrogen-containing oral contraceptives Estrogens (oral) Heroin/methadone 5-Fluorouracil Mitotane Tamoxifen |
These drugs may increase serum thyroxine-binding globulin (TBG) concentration. |
| Androgens/anabolic steroids Asparaginase Glucocorticoids Slow-release nicotinic acid |
These drugs may decrease serum TBG concentration. |
Potential impact (below): Administration of these agents with Synthroid results in an initial transient increase in FT4. Continued administration results in a decrease in serum T4 and normal FT4 and TSH concentrations.
| Salicylates (>2 g/day) | Salicylates inhibit binding of T4 and T3 to TBG and transthyretin. An initial increase in serum FT4 is followed by return of FT4 to normal levels with sustained therapeutic serum salicylate concentrations, although total T4 levels may decrease by as much as 30%. |
Other Drugs:
|
These drugs may cause protein-binding site displacement. Furosemide has been shown to inhibit the protein binding of T4 to TBG and albumin, causing an increase free T4 fraction in serum. Furosemide competes for T4-binding sites on TBG, prealbumin, and albumin, so that a single high dose can acutely lower the total T4 level. Phenytoin and carbamazepine reduce serum protein binding of levothyroxine, and total and free T4 may be reduced by 20% to 40%, but most patients have normal serum TSH levels and are clinically euthyroid. Closely monitor thyroid hormone parameters. |
See the full Prescribing Information for additional information - Section 7.0 for drug interactions.
Drugs that may alter hepatic metabolism of T4 (hypothyroidism)
Potential impact: Stimulation of hepatic microsomal drug-metabolizing enzyme activity may cause increased hepatic degradation of levothyroxine, resulting in increased Synthroid requirements.1
| Drug or Drug Class | Effect |
|---|---|
| Phenobarbital Rifampin |
Phenobarbital has been shown to reduce the response to thyroxine. Phenobarbital increases L-thyroxine metabolism by inducing uridine 5’-diphospho-glucuronosyltransferase (UGT) and leads to lower T4 serum levels. Changes in thyroid status may occur if barbiturates are added or withdrawn from patients being treated for hypothyroidism. Rifampin has been shown to accelerate the metabolism of levothyroxine. |
Drugs that may decrease conversion of T4 to T3
Potential impact: Administration of these enzyme inhibitors decreases the peripheral conversion of T4 to T3, leading to decreased T3 levels. However, serum T4 levels are usually normal but may occasionally be slightly increased.1
| Drug or Drug Class | Effect |
|---|---|
| Beta-adrenergic antagonists (eg, propranolol >160 mg/day) | In patients treated with large doses of propranolol (>160 mg/day), T3 and T4 levels change, TSH levels remain normal, and patients are clinically euthyroid. Actions of particular beta-adrenergic antagonists may be impaired when a hypothyroid patient is converted to the euthyroid state. |
| Glucocorticoids (eg, dexamethasone ≥4 mg/day) | Short-term administration of large doses of glucocorticoids may decrease serum T3 concentrations by 30% with minimal change in serum T4 levels. However, long-term glucocorticoid therapy may result in slightly decreased T3 and T4 levels due to decreased TBG production (see above). |
Other drugs:
|
Amiodarone inhibits peripheral conversion of levothyroxine (T4) to triiodothyronine (T3) and may cause isolated biochemical changes (increase in serum free T4, and decreased or normal free-T3) in clinically euthyroid patients. |




